Interpret best liver health indexes and biomarkers against optimal ranges, automatically generating differential diagnoses and pinpointing the source of enzyme abnormalities. It offers recommendations informed by clinical guidelines and optional AI-driven detection of rare conditions beyond conventional screenings.
Open in Browser for Full Features
Access interactive features, detailed explanations, and AI interpretations.
If printed on paper
Scan with Phone
If this is a PDF document
Click or copy-paste the link
(this usually does not work, use QR code)
🔒 100% Private - No data leaves your computer after opening
Enter values
all fields are optional
Result summary
This tool is for informational purposes only and not intended for diagnosis.
Fatty liver
Enter values to interpret
Liver fat (steatosis) is the accumulation of triglycerides within liver cells (hepatocytes). It's very common and is often driven by obesity, insulin resistance, or alcohol use.
Liver scarring
Enter values to interpret
Liver fibrosis is the excessive build-up of scar tissue in response to chronic liver injury. It's most often driven by long-standing inflammation from causes such as viral hepatitis, persistent alcohol use, or severe NAFLD.
Recommended actions
Enter values to interpret
Differential Diagnosis Calculations
ANI: 000
ALD/NAFLD Index is used for distinguishing Alcoholic from Nonalcoholic Fatty Liver Disease.
To calculate ANI, enter values for: Gender, Weight, Height, AST, ALT, MCV.
- < -2.2 - NAFLD
- -2.2 - 2.2 - Mixed
- > 2.2 - ALD
Probability of Alcoholic Liver Disease:
000%
ANI is useful if patient's alcohol consumption history is unclear or deemed unreliable. Short-term abstinence (few months) does not significantly alter the ANI.
It is crucial to exclude other potential causes of liver disease before applying the ANI.
R-Factor: 000
R-Factor is used for distinguishing acute liver injury (Hepatocellular from Cholestatic). Often used when drug induced liver injury (DILI) is suspected.
- < 2 - Cholestatic
- 2 - 5 - Mixed
- > 5 - Hepatocellular
To calculate R-Factor, enter values for: ALT, ALP.
Cholestasis is seen in: Gallstones; Malignancy (pancreatic, cholangiocarcinoma); Primary Biliary Cholangitis (PBC); Primary Sclerosing Cholangitis (PSC), often associated with IBD;
Drugs associated with cholestasis: Amoxicillin-clavulanate; macrolides (erythromycin); trimethoprim-sulfamethoxazole; anabolic steroids; combined oral contraceptives; chlorpromazine.
Mixed pattern / inconclusive.
If the presentation is not acute, this pattern is most often seen with fatty liver (NAFLD or alcohol-related).
A hepatocellular pattern is seen in: Viral Hepatitis or other viral infections; Autoimmune hepatitis; ischemic “shock” liver; Wilson's disease, hemochromatosis, alpha-1 antitrypsin deficiency; Toxin exposure; Budd-Chiari syndrome
Drugs associated with hepatocellular pattern: Acetaminophen (paracetamol); statins; certain antibiotics (e.g., isoniazid, nitrofurantoin); antiepileptics (e.g., valproate, phenytoin); NSAIDs (e.g., diclofenac); methotrexate; amiodarone; herbal/dietary supplements.
D/T Bilirubin Ratio: 000
The D/T ratio is used to differentiate between different types of jaundice and liver injury patterns.
- < 0.2 - Pre-hepatic
- 0.2 - 0.5 - Hepatocellular
- > 0.5 - Cholestatic
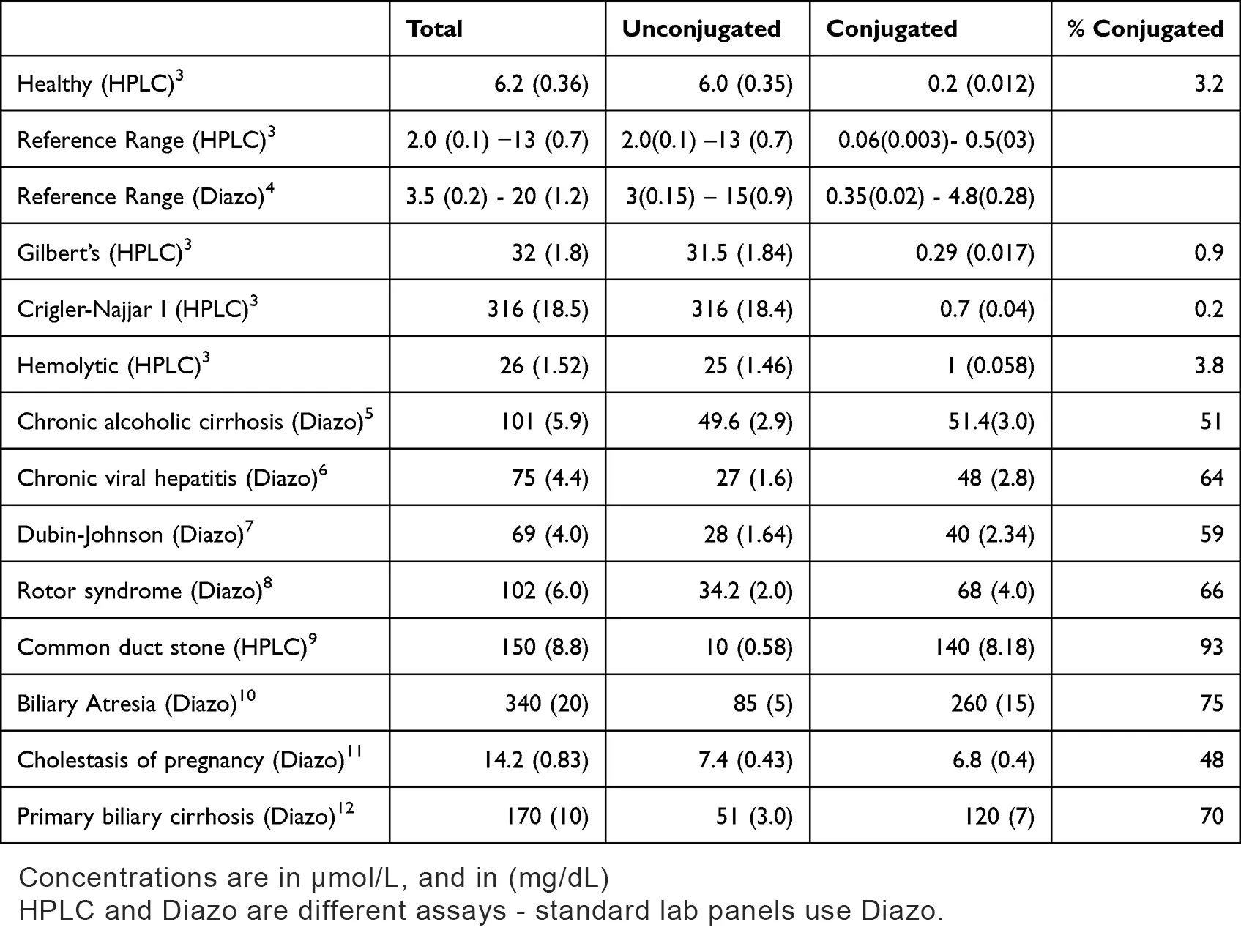
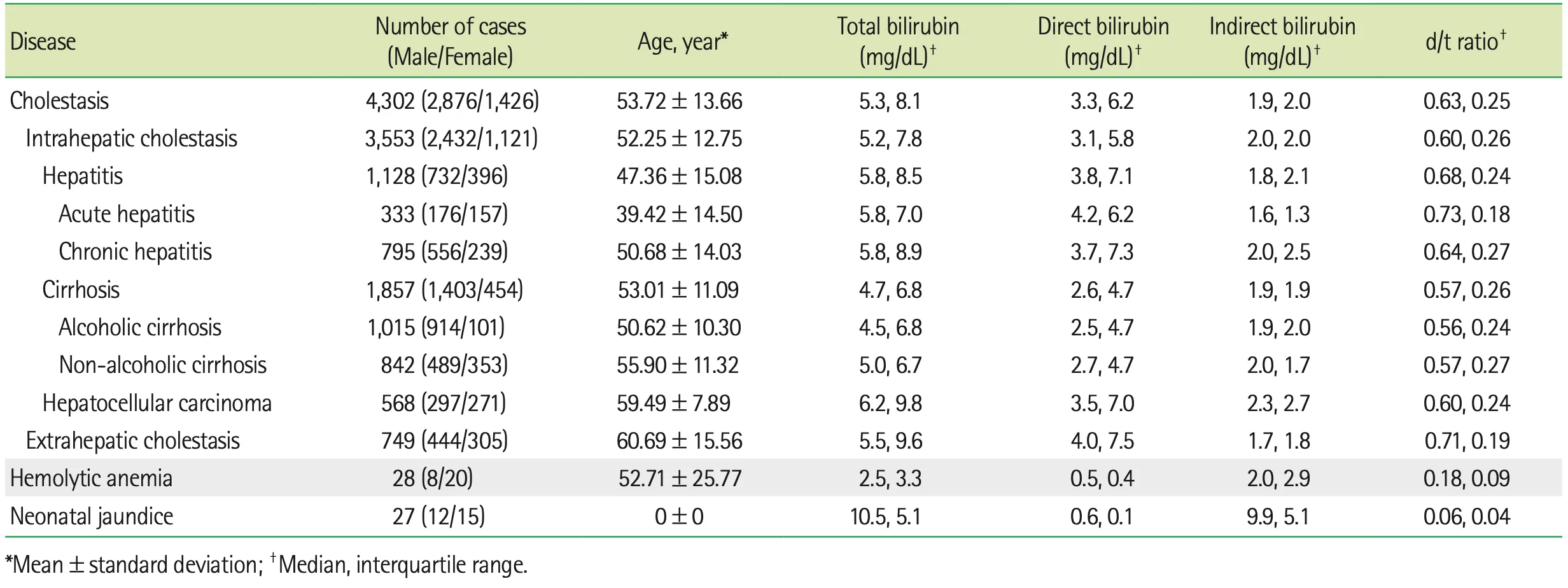
To calculate D/T Bilirubin Ratio, enter values for: Bilirubin (Direct), Bilirubin (Total).
Pre-hepatic pattern - mostly unconjugated bilirubin. The liver is conjugating normally; excess comes from over-production.
Pre-hepatic pattern is most commonly seen in hemolytic processes (e.g., autoimmune hemolytic anemia, transfusion reactions) and benign unconjugated syndromes (Gilbert's syndrome).
Hepatocellular injury pattern - both conjugation and canalicular export partly impaired.
Hepatocellular pattern is mostly seen in acute viral hepatitis or toxin/alcohol-related hepatocellular damage.
Cholestatic / obstructive pattern - predominantly conjugated bilirubin. Bilirubin is conjugated but can’t reach the gut.
Cholestatic pattern is most commonly seen in extra-hepatic biliary obstruction, like in choledocholithiasis; malignancy or less frequently intra-hepatic cholestasis.
Your
D/T Bilirubin Ratio
is optimal
Hepatic steatosis | Fatty liver disease | NAFLD | NASH
TyG-BMI: 000
Triglyceride-Glucose index multiplied by BMI is one of the best models to predict NAFLD.
To calculate TyG-BMI, enter values for: Weight, Height, Triglycerides, Glucose.
- yellow - NAFLD possible
- red - NAFLD likely
FLI: 000
Fatty Liver Index is one of the best models to predict liver fat content.
To calculate FLI, enter values for: Weight, Height, Waist circumference, Triglycerides, GGT.
Gender is required to interpret FLI.
- yellow - Fatty liver possible
- red - Fatty liver likely
Hepatic fibrosis | Liver scarring
FIB-3: 000
The Fibrosis-3 Index is an improved version of the FIB-4, that does not include age. It outperforms both FIB-4 and APRI.
To calculate FIB-3, enter values for: AST, ALT, PLT.
- yellow - F2 or higher fibrosis possible
- red - F3 or higher fibrosis possible
LSS: 000
Liver stiffness score is currently one of the best models to predict liver fibrosis. Outperforms FIB-4, APRI and HSI. Trained on NHANES dataset.
To calculate LSS, enter values for: Weight, Glucose, AST, PLT, Albumin.
- yellow - F2 or higher fibrosis possible
- red - F2 or higher fibrosis likely
Probabilities of having different fibrosis stages:
Stage F2 fibrosis is fully reversible, Stage F3 is partially reversible, and Stage F4 is largely irreversible.
Individual biomarkers
Plots show optimal ranges; values above the UNL are displayed as multiples (xUNL).
AST: 000 IU/L
Transaminase released from hepatocytes and cardiac/skeletal muscle (with minor contributions from kidney, pancreas, brain, RBCs and gallbladder).
Enter value for AST to interpret.
Low AST levels are usually not concerning. However, they may indicate Vitamin B6 Deficiency, End-Stage Liver Disease (Cirrhosis), uremia, diabetic ketoacidosis, and pregnancy.
Sources: optimaldx,selfdecode
Mixed pattern / inconclusive
Elevated AST levels are seen in muscle injury (e.g., strenuous exercise, seizures, myopathies, myocardial infarction or heart failure), tissue damage (severe burns, surgery), liver injury (fatty liver, viral or other infections, malignancy), anorexia or rapid weight change (e.g., >5 kg/week), pancreatitis, gallbladder attack and hemolysis (e.g., hemolytic anemia, splenomegaly).
Several drugs can increase AST including: chronic alcohol, NSAIDs, acetaminophen, oral contraceptives, statins, certain antibiotics, corticosteroids, toxins like lead, mercury, and pesticides.
Sources: wikipedia,optimaldx,selfdecode
ALT: 000 IU/L
Highly liver-specific transaminase, but with minor contributions from skeletal and cardiac muscle, pancreas, and gut.
Enter value for ALT to interpret.
Low ALT levels are associated with low muscle mass (e.g., elderly, frail), Vitamin B6 Deficiency, Chronic Kidney Disease, CVD and cancer mortality in the elderly.
Sources: optimaldx,selfdecode
Mixed pattern / inconclusive
ALT is highly specific to liver injury (Fatty liver, Viral hepatitis, Autoimmune hepatitis, Liver cancer, Alcohol liver damage, Mononucleosis, Hemochromatosis).
Muscle damage – strenuous exercise, trauma, myocardial infarction, congestive heart failure.
Gallstones; Biliary disease; pancreatitis; both obesity and anorexia; rapid weight change; celiac disease; hemolysis.
Many toxins and drugs can increase ALT, but most notable are: Paracetamol, NSAIDs, statins, phenytoin, allopurinol, and antibiotics, especially amoxicillin.
Sources: wikipedia,optimaldx,selfdecode
ALP: 000 IU/L
Alkaline phosphatase is primarily released from the bile ducts and bone. Minor sources include the intestinal mucosa, kidneys, and placental tissue (during pregnancy).
Enter value for ALP to interpret.
ALP is seen decreased in Malnutrition (insufficient calories or very low protein diet), Magnesium or Zinc Deficiency, advanced liver disease, Hypothyroidism, severe anemia, excess cortisol levels and more.
Medication that can decrease ALP levels: mega-dosing vitamins D or B, Hormone replacement therapy, oxalates, nitrofurantoin, Cinacalcet and more.
Sources: optimaldx,selfdecode,xiahepublishing
Mixed pattern / inconclusive
Cholestatic liver injury – biliary obstruction, acute cholecystitis, cholangitis, cirrhosis, hepatic tumors.
Bone/osteoblastic activity – Paget’s disease, osteomalacia/rickets, fracture healing, growth spurts, hyperparathyroidism, bone metastases.
Gut/intestinal mucosa issues – IBS, celiac disease, intestinal ischemia; kidney disease; various malignancies; vitamin D deficiency; hyperthyroidism; rheumatoid arthritis; sickle cell crises.
Medications – birth control pills, allopurinol, colchicine, antibiotics, fluorides, verapamil, nicotinic acid, vigorous exercise.
Sources: wikipedia,optimaldx,selfdecode
GGT: 000 IU/L
Serum Gamma-glutamyl transferase usually originates from hepatocytes and cholangiocytes (plus pancreas).
Enter value for GGT to interpret.
Low GGT levels are usually not concerning. However, they may indicate Acute intrahepatic cholestasis, Hypothyroidism, magnesium deficiency or vitamin B6 deficiency, bone disease (low bone mass density).
Drugs that can cause low GGT: Fibrate Drugs (Clofibrate, Fenofibrate), Estrogen-Containing Medications,milk thistle, antioxidants.
Sources: optimaldx,xiahepublishing
Mixed pattern / inconclusive
Major serum GGT contributors: Liver (both hepatocytes and cholestasis), gallbladder, pancreas and kidneys. Also increased in insulin resistance, toxin exposure, oxidative stress and increased antioxidants (glutathione) need etc.
Drugs that can increase GGT: Alcohol, anti-seizure medications and more.
Sources: optimaldx,selfdecode
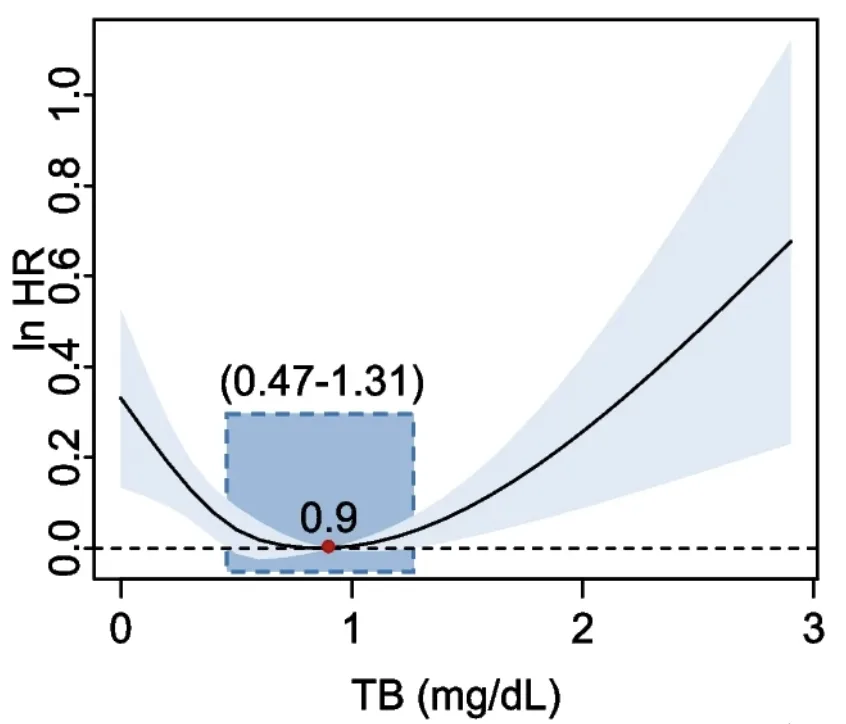
Bilirubin (Total): 000 mg/dL
Heme-catabolism end-product processed by the liver and excreted in bile, reflecting hemolysis and hepatic clearance.
Enter value for Bilirubin (Total) to interpret.
Low total bilirubin is associated with systemic inflammation, oxidative stress, stroke, increased carotid intima-media thickness, arterial stiffness, diabetic peripheral neuropathy, metabolic syndrome, and Chronic Kidney Disease.
Drugs that can decrease bilirubin levels: smoking, caffeine, barbiturates, penicillin, and large doses of salicylates.
Sources: optimaldx,selfdecode
Mixed pattern / inconclusive
High total bilirubin is associated with liver dysfunction, hepatitis, Gilbert’s Syndrome, Strenuous Exercise, Gallstones and Gallbladder Disease, Pancreatitis, Appendicitis, obstruction of extrahepatic ducts, RBC hemolysis.
Sources: optimaldx,selfdecode
Your
Bilirubin (Total)
is optimal
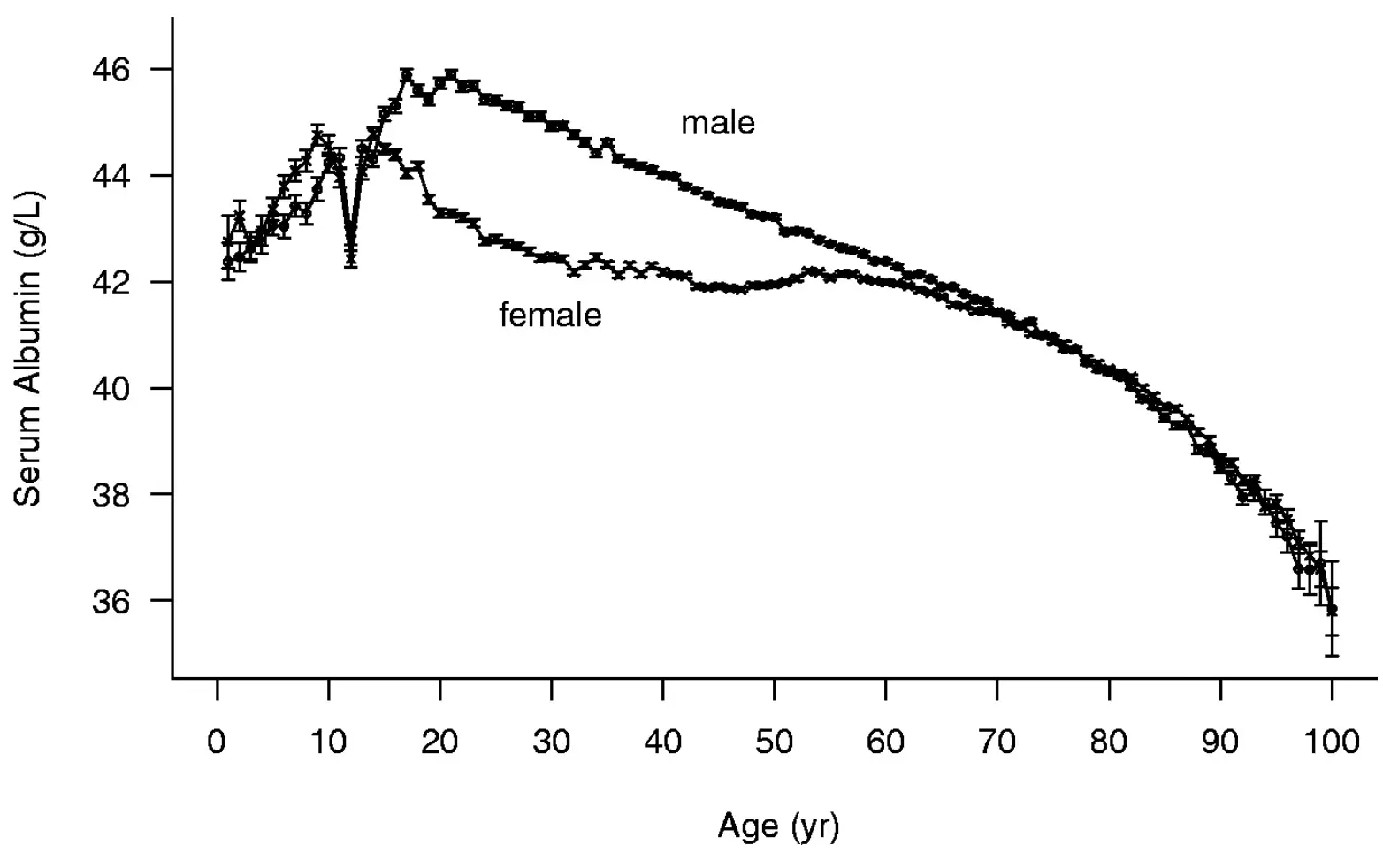
Albumin: 000 g/dL
Principal liver-synthesized plasma protein maintaining oncotic pressure and ferrying hormones, drugs and nutrients.
Enter value for Albumin to interpret.
Low albumin is primarily a consequence of illness rather than a cause, and it serves as a late-stage indicator of inflammation. It is frequently observed in chronic or persistent inflammatory states.
Low albumin is also associated with liver disease, kidney disease, diabetes, heart failure, fluid overload, advanced malnutrition (particularly from protein deficiency or malabsorption), severe burns, and occasionally cancer.
Sources: selfdecode,optimaldx
Mixed pattern / inconclusive
Elevated albumin levels occur with dehydration (commonly due to vomiting or diarrhea) and insulin resistance.
Sources: selfdecode,optimaldx
Why this beats ChatGPT
All research is done by humans. AI was only used to refine the writing for better readability.
Optimal ranges, not just “normal”
Generic AI uses normal lab ranges (based on population averages). This tool uses functional, best-outcome targets.
Evidence-locked math. Not hallucinations
Generic AI chatbots don’t know which calculated indices are best or their optimal cutoff values.
Clinically significant differentials
We run relevant differential diagnosis calculations, but only when it's clinically significant.
Privacy by default
Everything happens in your browser and no personal or medical information leaves your computer.
Special Thanks to the Following Researchers and Doctors
I extend my gratitude for their invaluable consultation during the development of this Liver Function Blood Test Interpreter tool.
Kazuya Kariyama, M.D., Ph.D.
Deputy Hospital Director at Okayama City Hospital, Department of Gastroenterology.
Dr. Kariyama is the inventor of the FIB-3 index and provided valuable insights into its cut-off values and clinical application.
Prof. Hongbing Sun, Ph.D.
Department of Chemistry, Biochemistry, and Physics, Rider University.
Prof. Sun is the inventor of the LSS index and contributed valuable insights into its calculation, interpretation, and optimal cut-off values.
Dr. Luis E. Simental Mendía, Ph.D.
Biomedical Research Unit, Mexican Institute of Social Security.
Dr. Simental's research focuses on obesity-related metabolic disorders. He is the inventor of the TyG index and provided expert consultation on its calculation and application.

About the site author
My personal mission is to extend human lifespan by collectively adding 1 million years to people's lives.
That’s why I made this site 100% free—no sign-up, no email. Just instant results.
Zsolt Szabo
Precision Health Consultant for Longevity Clinics, Biohacker, and Software Engineer
How would you improve this tool ?
Any feedback is welcome at
.