Introduction
Myopia is the most common ocular disease affecting public health worldwide. It is predicted that by 2050, half of the world’s population will be nearsighted, and nearly 10% of people will have high myopia [1]. It has been found that the ratio of students with myopia ranges from 80% to 90% in East Asia, where myopia is particularly prevalent [2]. Myopia, especially high myopia, leads to various blinding eye disease such as macular degeneration, glaucoma, retinal detachment, and is one of the most important ringleaders of blindness [3]. Therefore, the serious social burden caused by myopia has attracted widespread attention [1].
It is widely known, behaviors such as near work and indoor activities are closely correlated with myopia [4]. Since 2019, COVID-19 began to wreak havoc globally. During this period, a degree of home restriction and online teaching were implemented nationwide, which resulted in reduced outdoor activities, increased near work and more usage of electronic devices in children and adolescents [5], and thus brought more progression of myopia and greater increments of AL, unsurprisingly [6,7,8,9,10]. However, the extent of these affected patterns was unstable due to the non-mandatory nature of the restrictions and policy instability. As a result, the degree of these affected habits was unstable during most of this period, introducing potential confounding variables into the related research. Shanghai continued in dynamic zero-COVID policy until 2022. Due to the epidemic outbreak in February 2022, Shanghai had to switch the policy to static lockdown citywide until lift of the lockdown in June 2022 [11]. Certainly, this tactic had a certain effect on the spread of COVID-19, as all residents of shanghai, including school-age children, had to be blocked at home, and all students had to receive thoroughly online learning. Throughout this entire period, every school-age child had nearly identical habit and eye usage habits and duration, without any outdoor activities. This strict strategy, which involved such a wide range of population across the whole city and lasted for such a long time, only occurred during the static lockdown phase in Shanghai from February to June 2022 [12]. This phase did not occur in other cities or periods, providing an excellent precondition for controlling variables in the research of myopia.
Methods such as atropine, defocus spectacle lens and orthokeratology have become commonly-used strategies [13, 14]. Previous studies indicated that low-concentration atropine can reduce the myopia development, which was accelerated by home confinement and increased near work during the pandemic [15]. As another method, orthokeratology was proven to not only control the progression of myopia more effectively [16, 17], but also lead children to better psychological and behavioral performance, compared to wearing common framed eyewear [18, 19].
However, until now, it is still underexplored whether orthokeratology can achieve the same control effect of myopia under adverse conditions, such as excessive near work and lack of outdoor activities. Therefore, in our study, we longitudinally compared the differences in increments of AL between children who use orthokeratology before, during and after the lockdown period, and conducted a horizontally comparison between children with and without orthokeratology. The purpose of this study is to investigate the effect of orthokeratology in a high-risk environment during the period of home confinement in COVID-19, Shanghai.
Method
Participants and study design
In this retrospective study, all cases were collected from the outpatient of Shanghai Eye Disease Prevention and Treatment Center & Shanghai Eye Hospital. The experimental group (patients with orthokeratology) was from June 2021 to October 2021 and the control group (patients without orthokeratology) was in February 2022.
Experimental group inclusion criteria: (1) Ages 7–18 years old; (2) Diagnosed as monocular or binocular myopia after cycloplegic optometry objectively, with best corrected visual acuity ≤ 0.00 log of minimum angle of resolution (log MAR) units (Snellen equivalent, 20/20); (3) Met the eligibility criteria for orthokeratology as determined by ophthalmologist (myopia of -0.75 to -7.00D and astigmatism of 0 to 1.5D); (4) Had been wearing lenses for at least 1 year before February 2022(last follow-up before the lockdown) and continued wearing at least 6 months later after the lockdown was lifted; (5) Wore lenses for more than 95% of the duration within each phase; (6) AL Measuring with IOLMaster without missing any follow-up.
Exclusion criteria (1) Cessation of orthokeratology for any reason; (2)History of ocular surgery during any phase; (3) Any ocular disease likely to affect orthokeratology or the accuracy of AL measurement; (4) No use of other myopia control methods in combination, such as atropine.
Only the parameter of one eye were included. Ipsilateral eye is included when wearing lens unilaterally, and the right eye was included when wearing bilaterally.
A total of 139 myopic children, 139 eyes with orthokeratology, were included in this study from June 2021 to October 2021. Among them, 128 children used orthokeratology bilaterally, while 11 children used it unilaterally.
Additionally, 91 myopic children, 91 eyes, met the inclusion criteria (1) ~ (3) without orthokeratology, were included as a horizontal comparison during the epidemic (these myopic children were preparing to use orthokeratology but did not acquire lens before the home confinement period in time until lift of the lockdown).
The study was approved by the Institutional Ethics Committee of Shanghai General Hospital, Shanghai Jiao Tong University (No. [2020]093) and adhered to the tenets of the Declaration of Helsinki. In this study, only the clinical data of patients were retrospectively collected, and the requirement for informed consent was waived.
Orthokeratology selection and adaptation
The variety of orthokeratology lenses is not restricted and includes Lucid (Lucid, Korea), Euclid (Euclid Systems Corporation, USA), or CRT (Paragon, USA).
Trial lenses were selected based on the parameters from cycloplegic optometry and corneal topography. Then the lenses were worn at least 30 min. Final orthokeratology selection was based on observation and corneal fluorescence results under the slit lamp, optometry with lenses, and corneal topography after removal. After delivery of the lenses, a manual on lens cleaning and maintenance was also provided to the parents of these children.
Axial length measurement and normalize
AL was measured by IOLMaster (Carl Zeiss Meditec AG, Jena, Germany) every 6(± 2) months, using an automatic scanning pattern. Five valid data points were selected and the average was taken as the final result.
Our primary outcome was the change in AL, which was proportionally adjusted to the AL growth every 6 months to normalize the nonuniform periods caused by COVID-19 home confinement.
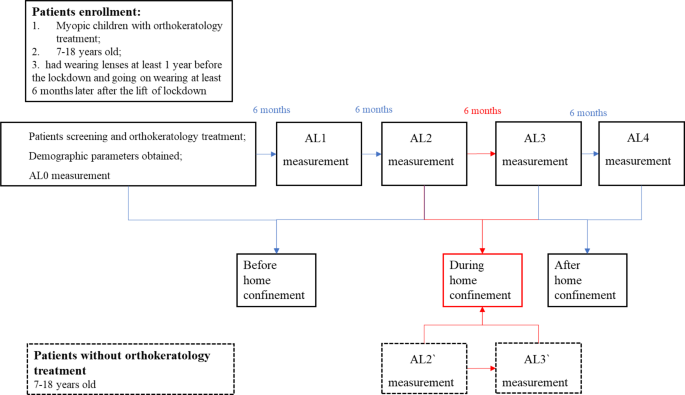
Measurements were taken at five time points for children with orthokeratology and two time points were measured in the non-wearing children. AL0, AL1, AL2, AL3 and AL4 were defined as the AL examined at the follow-up before first wearing Ortho-K, 6 months after, before the home confinement period, after the home confinement period and the last follow-up (6 months after the lifting of lockdown), respectively. Therefore, during home confinement period was between AL2 and AL3. AL2` and AL3` was defined as before, and after home confinement period in the children without Ortho-K.
The study design is shown in Fig. 1.
Study design. The research retrospectively enrolled myopic children applying the OK treatment. The axial length (AL) measurements before first wearing (AL0), 6 months after (AL1), before home confinement period (AL2), after home confinement period (AL3) and the last follow-up (AL4), respectively. Patients without orthokeratology treatment was enrolled only before home confinement period (AL2`) and after home confinement period (AL3`)
Statistics
The data were analyzed using SPSS 22.0. The variations of AL every 6 months were the main outcome. The normality of each variable was examined with the Shapiro test. Continuous variables were expressed as mean ± SD. The difference in AL increments before, during and after home confinement every 6 months were analyzed with One-way ANOVA. The Bonferroni correction was used for post hoc analysis when performing multiple comparisons. Correlation analysis was performed to explore the factors influencing the increments of AL during home confinement, including age, gender, baseline SE and baseline AL. Subgroup analysis was performed in patients aged ≤ 10 years or > 10 years and in spherical equivalent (SE) ≤ 300 or > 300. Excessive AL growth was defined as ≥ 0.1 AL growth every 6 months and < 0.1 as negative. Numeration data were compared between groups using Chi-square test. The statistical significance threshold was set at p < 0.05.
Result
The demographic parameters for included subjects (experimental group, N = 139; control group, N = 91) are shown in Table 1. The mean age was 10.50 ± 1.80 years and 10.61 ± 1.89 years in the experimental group and the control group, respectively; The mean spherical equivalent was − 2.82 ± 1.13 diopters and − 3.04 ± 1.33 diopters, respectively.
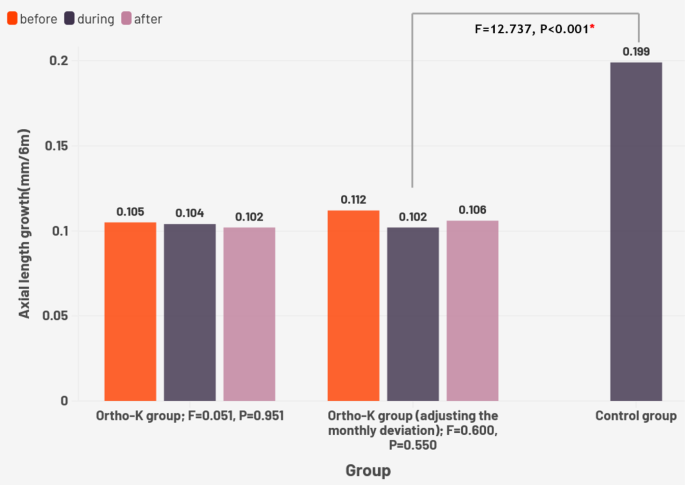
The AL growth before, during, after home confinement is showed in Fig. 2. In the experimental group, the AL growth was 0.105 ± 0.093 mm/6 months, 0.104 ± 0.107 mm/6 months and 0.102 ± 0.078 mm/6months before, during and after home confinement, respectively. The time interval was 5.64 ± 1.33 month, 5.98 ± 1.13 month and 5.96 ± 1.17 months before, during and after home confinement, respectively. There were no significant differences in the AL growth (F = 0.051, P = 0.951) or AL growth adjusting for the monthly deviation (F = 0.600, P = 0.550), either. During home confinement, school-age children who underwent orthokeratology had an axial growth of 0.102 ± 0.105 mm/6months compared to 0.199 ± 0.165 mm/6months without (F = 12.737, P = 0.000).
Influence factors for per 6-month AL growth during home confinement were analyzed in the experimental group, and the results are shown in Table 2. During home confinement, age was significantly negatively related to monthly AL growth (P = 0.007) and SE baseline showed a weak correlation to it (P = 0.027), while gender (P = 0.603) and baseline AL (P = 0.208) were not significant. The result remained the same when adjusting for the monthly deviation.
During home confinement, a subgroup analysis of AL growth (mm/6m) between the Ortho-K group and control group is shown in Table 3. Myopia control rate (MCR) of all participants, < 10 years old subgroup, ≥ 10 years old subgroup, SE > 3.00 subgroup and ≤ 3.00 subgroup were 48.7%, 50.7%, 48.3%, 58.6% and 43.4%, respectively. (myopia control rate = change in AL in the control group - change in AL in the Ortho-K group/change in AL in the control group). Each P value for subgroups between the Ortho-K group and the control group was < 0.001. There was no significant difference in MCR between age groups (F = 1.588, P = 0.209), neither between different degree of myopia (F = 0.759, P = 0.385).
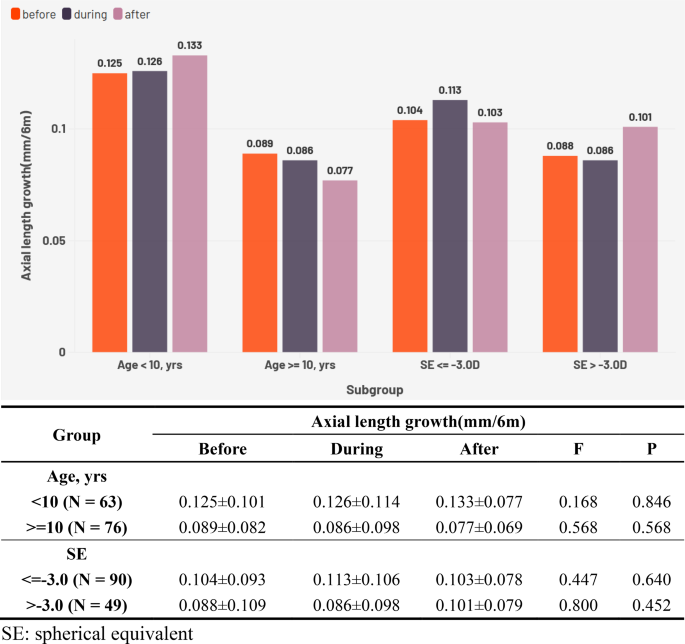
The results of subgroup analysis in the experimental group are demonstrated in Fig. 3. For younger children (≤ 10 yrs, average8.89 ± 0.86 yrs), every 6-month AL growth before, during, and after home confinement was 0.125 ± 0.101 mm/6m, 0.126 ± 0.114 mm/6m, and 0.133 ± 0.077 mm/6m, respectively. For older children (> 10 yrs, average11.85 ± 1.25 yrs), before, during, and after home confinement every 6-month AL growth was 0.089 ± 0.082 mm/6m, 0.086 ± 0.098 mm/6m, and 0.077 ± 0.069 mm/6m, respectively. These values were 0.104 ± 0.093 mm/6m, 0.113 ± 0.106 mm/6m, and 0.103 ± 0.078 mm/6m for lower SE (≤ -3.0D, average − 2.13 ± 0.56D); and 0.088 ± 0.109 mm/6m, 0.086 ± 0.098 mm/6m, and 0.101 ± 0.079 mm/6m for higher SE (>-3.0D, average − 4.09 ± 0.76D), respectively.
There were no significant differences in the AL growth before, during and after home confinement in younger children (P = 0.846), older children (P = 0.568), lower SE (P = 0.640) and higher SE (P = 0.452) subgroups, respectively.
An annual increase of less than 0.2 mm in the AL of school-age children is considered a good responder to the control strategy [20]. Therefore, we used a < 0.1 mm growth of AL half a year as the boundary for a good responder for statistics. The result of χ2 tests showed that there was no significant difference in the proportion of AL growth before, during and after home confinement (P = 0.662) in the experimental group, as shown in Table 4. When conducting subgroup analysis, there were no significant differences in higher SE (P = 0.702), lower SE (P = 0.393), younger children (P = 0.745) and older children (P = 0.710) subgroups, respectively. Also, no significant differences were found when adjusting for the monthly deviation, as shown in Table 5.
Discussion
In this study, we explored the effect of orthokeratology on myopia control under the strict home confinement policy in Shanghai in 2022, which was implemented due to the Covid-19 pandemic. Our findings showed no significant progression of myopia in school-age children undergoing orthokeratology during this period when compared to pre- and post-lockdown period. This suggests that orthokeratology remains effective in controlling myopia even under challenging conditions.
Over the past few decades, with an unrelenting pace of growth in myopia and high myopia worldwide, the incidence of many ocular diseases has also shown a simultaneous increase, subsequently bring more blindness caused by high myopia [3]. As a result, myopia has become the focus of global concern for health and hygiene [1]. In China, the prevalence of myopia is notably high, and display an age-lowering trend [21]. Additionally, the earlier myopia appears, the greater the risk of high myopia in the future [22]. In response to this growing concern, the Chinese Ministry of Education released the “Suitable Technical Guidelines for Myopia Prevention and Control in Children and Adolescents” [4] and updated it in 2021. This guideline aims to curb the progression of myopia earlier. Among the recommended strategies for myopia control, orthokeratology plays one of the pivotal roles. Furthermore, the guidelines emphasize the importance of increasing outdoor activities and reducing near work as crucial measures to slow myopia progression.
Previous studies have shown that strategies such as low-concentration atropine can help reduce the progression of myopia, which was accelerated by home confinement and increased near work during the pandemic [15]. Orthokeratology, as an alternative method for myopia control, has demonstrated superior effective compared to low-concentration atropine [23, 24]. This led to the scientific question of our study: Can orthokeratology also retard the myopic progression under such disadvantageous environment. Our results indicate that, even under extreme conditions such as a lack of outdoor activities, increased near work and more time spent on electronic devices, orthokeratology continues to show positive effects on myopia control. During the period of strict home confinement, school-age children undergoing orthokeratology exhibited a slower axial growth of 0.102 ± 0.105 mm/6months, compared to 0.199 ± 0.165 mm in those not receiving orthokeratology, as shown in Fig. 2. This demonstrates the positive impact of orthokeratology on myopia control. The AL growth was 0.105 mm/6months before, 0.104 mm/6months during, and 0.102 mm/6months after the home confinement period, with on significant difference (P > 0.05). This suggests that strict home confinement during the pandemic did not lead to accelerated AL growth in children who underwent orthokeratology, as depicted in Fig. 2. Furthermore, factors such as age and diopter did not impact the efficacy of orthokeratology, indicating that Ortho-K could be a potential better treatment for children in high-risk environments, as shown in Fig. 3.
Previous research has demonstrated that orthokeratology significantly controls the growth of AL [25]. A recent meta-analysis revealed that, compared to 0.22–0.36 mm AL elongation annually before the epidemic, this figure raised to 0.29 to 0.44 mm during the epidemic [26]. In contrast, individuals without any control strategy, the annual increments of AL decreased from 0.4 to 0.5 mm to 0.2–0.3 mm following orthokeratology treatment [27]. In our study, the use of orthokeratology reduced the AL growth from 0.199 to 0.102 mm over a 6-month period during home confinement, as shown in Table 3. The findings reported in previous studies align with ours.
Additionally, although SE baseline and AL growth showed a weak correlation, we observed that the proportion of school-age children showing good responder (< 0.1 mm growth of AL) did not significantly decrease under the strict home confinement after using orthokeratology, regardless of the children`s age or myopia degree, as shown in Table 4.
Based on the results above, it can be suggested that orthokeratology maintained a moderate and stable effect on myopia control even under disadvantageous environment of home confinement during the epidemic. For this phenomenon, several potential explanations can be speculated to account.
Firstly, past research has shown that school-aged children experienced longer sleep during home confinement compared to their offline learning period before the confinement [28]. With longer sleep, a more sufficient defocus ring of orthokeratology may form, potentially enhancing the effectiveness of myopia control. Therefore, we speculate that the increased sleeping hours during the pandemic could contribute to a slower increment in AL for those undergoing orthokeratology. This positive effect may help offset the negative impact of poor eye-care habits caused by the extended home confinement.
Secondly, this phenomenon described above may be attributed to the overwhelming effects of orthokeratology in controlling myopia, which appears to counteract the negative impact of reduced outdoor activities and increased near work. Given the developmental characteristics of myopia, age has been proven as an independent risk factor for its progression, with younger children exhibiting a faster growth rate of AL compared to their older counterparts [29]. In addition, younger were found to be more susceptible to myopia progression during the Covid-19 home confinement period [30]. Our study showed that MCR for orthokeratology during this period was 48.7%, which align with the 47% − 64% range of MCR reported in other studies [17]. Moreover, there was no significant difference in the results across subgroups based on age, as shown in Table 3. The data suggests a tendency that the faster myopia progressed brought by lower age, the better control rate when using orthokeratology. This evidence moderately supports the hypothesis that orthokeratology can overcome extreme adverse conditions and effectively manage myopia. However, the lack of relevant research highlights the need for further studis in the future.
As an added note, in our results, the increase in AL at the first 6 months of orthokeratology use (0.063 ± 0.169) was significantly lower compared to the following 18 months (0.105 ± 0.093 mm/6 month before, 0.104 ± 0.107 mm/6 month during, and 0.102 ± 0.078 mm/6 month after the epidemic), as detailed in Appendix 1. A study by Wang’s et al. found that many children experienced a shortening of AL in the first month of using orthokeratology, followed by an increase in AL until it approaches baseline by the 7th month of lens wear [31]. This phenomenon is likely attributed to corneal flattening and choroidal thickening, leading to a temporarily shorter AL outcome [31]. Since the focus of our study was on the impact of strict home restrictions and changes in eye-care habits during the epidemic on AL control with orthokeratology in school-age children, the initial shortening of AL during the first 6 months could potentially confound our results. To address this, we excluded the data from the first 6 months of orthokeratology use and focused our analysis on the 6 months before, during, and after the epidemic. However, it is noteworthy that wang`s et al. suggested that the extent of initial axial control effect of orthokeratology may serve as a predictive indicator for its long-term myopia control effectiveness [31]. In our study, we observed that the control effect in the first 6 months also demonstrated a degree of predictability for subsequent myopia control, even under high-risk conditions, as shown in Appendix 2.
There were some limitations in our study. First, we did not administer a lifestyle questionnaire, resulting in a lack of data on screen time, near-work activities, and sleep duration. This gap hinders comparability between these factors and myopia progression, despite the near-uniform lifestyle conditions during lockdown (e.g., all students had ≥ 7 h of daily screen time with no outdoor activity opportunities). We will incorporate validated questionnaires and wearable sensors in future studies to address this limitation; Additionally, we only collected data on children who did not use orthokeratology only during the period of home confinement, rather than before and after, which limits the ability to make a sufficient horizontal comparison. Despite these limitations, the scenario of restricted outdoor activities and the forced shift to online learning for school-age children is unique and is almost impossible to be replicated. After all, thus strict static lockdowns imposed by the epidemic are unlikely to occur again. Furthermore, for ethical reasons, it would be challenging to replicate the passive restriction of outdoor activities and the inadvertent increase in near work.
In summary
In summary, under the strict home confinement policy in Shanghai in 2022, caused by Covid-19, there was no significant increase in AL in school-age children using orthokeratology compared to the periods before and after the confinement. This suggests that, even under challenging conditions for myopia control, orthokeratology can still achieve effective results. Our findings provide a solid theoretical foundation for children with limited outdoor activities or increased near work, helping us to select the ideal tactic for myopia control. Furthermore, this research lays the groundwork for future studies exploring the relationship between sleep duration and quality and the effectiveness of orthokeratology in controlling myopia.